A day in the life of a workforce manager in healthcare: juggling data, people, and unexpected curveballs

Workforce management can feel like a solitary journey, even though you’re interacting with numerous people daily. You’re often the sole decision-maker, impacting the daily routines of many. It’s a delicate balance: you must be decisive and data-driven to meet operational delivery expectations, yet compassionate because you’re deeply intertwined with the personal lives of your workforce.
When things don’t go as planned, fingers often point our way, even when resource planning and scheduling aren’t the sole culprits. Attrition can skyrocket when team morale dips or if HR practices aren’t up to par. With so many unexpected moving pieces, it often felt like I was making educated guesses back then, hoping our forecasts aligned with reality. Can anyone else relate?
The big picture: planning ahead
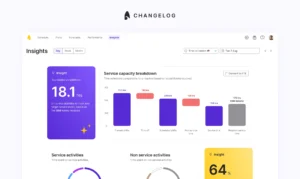
In my former role, I was fortunate that our BI platform was already synced with our product through advanced API integration. Our workforce management software was similarly integrated, allowing for seamless data flow. This setup provided me with a comprehensive overview of essential data insights such as hourly workforce supply breakdowns, the total number of patients addressed, queue times, disease distribution, and workforce utilisation right from our BI platform.
Using these insights, I typically planned 2-3 months ahead, determining the hourly supply needed for each service line for each clinical workforce type (different banding of nurses, GPs, advanced prescribers). If I foresaw a peak or quiet season, I factored in historical data on workforce and demand shrinkage, sudden workforce attrition, and other variables for capacity planning.
Our workforce was a blend of salaried and self-employed professionals. We prioritised salaried staff, aiming for a consistent rota. This meant that 60% of the rota was pre-planned 2-3 months in advance. The rest of the workforce would either fill in the gaps that were made visible to them or provide their availability, which I’d match with service demand requirements.
A typical “scheduling day”
Morning firefighting
Mornings often started with addressing urgent escalations and filling service gaps from last-minute cancellations. While we had a support pathway for volunteers and bank staff to cover these gaps, sometimes personal calls or enhanced rates were needed. The stakes were high in the healthcare industry; missing SLAs could mean patients went unseen or faced life-threatening situations. Balancing internal KPIs and business interests with the need for accuracy and focus was a daily challenge.
Analytics and forecasting
Once the fires were out, I dived into metrics, analytics, reporting, and forecasting. This provided a snapshot of recent events, how they might alter our forecasts, and whether we needed to pivot strategically.
Addressing workforce requests
Next, I tackled less urgent workforce requests. These could range from minor shift adjustments to more significant changes due to service alterations. Being data-driven helped me make informed decisions, and having numbers to back up responses could smooth over potential disagreements.
Strategic design and coordination
In that fast-paced environment, new partnerships and service lines were always emerging. On top of that, we had to staff for special unexpected services, such as clinical studies prompted by COVID. Patient behaviour could also shift dramatically due to unforeseeable national public health challenges. This meant aligning with the commercial team on SLAs, setting internal operational priorities, and coordinating with the recruitment team. It was crucial to ensure we had the right staff with the appropriate skills and on contract types that balanced the reliability of salaried employees with the flexibility of contractors and locums.
Speaking of recruitment, managing attrition was a constant challenge. This is especially in healthcare, where qualifications vary, coordinating weekly to align on recruitment goals was essential.
Reflections and moving forward
Looking back, the role of a healthcare workforce manager was a blend of challenges and rewards. Every day brought new puzzles to solve, from staffing unexpected services to navigating the ever-changing landscape of public health. But amidst the chaos, there were moments of clarity, where the right decisions led to improved patient care and a more efficient workforce.
Now, as part of the team at Surfboard, I’m channeling those experiences into creating workforce management software that make scheduling for support teams less solitary and more collaborative. Our aim is to humanise the workplace, alleviating some of the stresses that contribute to attrition. To all my fellow workforce managers and those in operations, here’s to the juggling act we perform daily – and to a future where we can make work more attuned to human needs.
If you’re in search of a no-code, ready-to-go scheduling solution that prioritises both operational efficiency and employee wellness, book a demo with our team.
Book a demo here